
It is possible that patients who are suffering from chronic pain respond differently to the different closure modalities given the underlying sensitized peripheral and central neuropathic pain pathways.
#Best spinal cord stimulator 2021 skin#
To our knowledge, there are no data directly comparing skin closure type for SCS and DRG-S surgeries. However, there may be differences related to a given specific surgical procedure. When these reviews are taken in sum, there is much conflicting data and no clear evidence as to the best technique. ĭata from other specialties have been published to look for differences in cosmesis, surgical site infection, and patient satisfaction between the two closure methods. Current specialty guidelines call for skin closure after implantation to be done with either subcuticular suture or staples as the existing evidence does not clearly support either method as superior.
National consensus guidelines have been published to report best practices related to the utilization of SCS and DRG-S therapies. Of course, these incisions require proper surgical closure to prevent wound breakdown, limit infection, and provide optimal postoperative cosmesis.
#Best spinal cord stimulator 2021 generator#
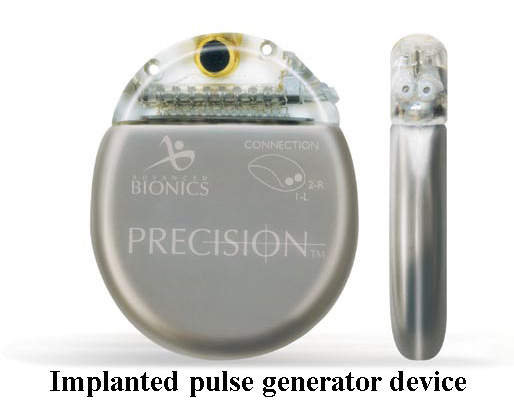
The surgical technique for implantation of a percutaneous SCS or DRG-S device generally involves the creation of multiple incisions: one utilized to insert and anchor the stimulating lead (s) and another to insert the implantable pulse generator (IPG). The expanding indications, progressive improvement in hardware, and development of new programming options have resulted in an increasing number of neuromodulation operations. Spinal cord stimulation (SCS) and dorsal root ganglion stimulation (DRG-S) are minimally invasive surgical approaches that are commonly used for certain refractory pain conditions. These findings are of interest to the pain practitioner and may be valuable in preoperative discussions with prospective patients. Increasing age was associated with decreased incisional pain scores at POD#10 ( β −0.06 (95% CI −0.09 to −0.03), ). Higher preoperative pain score ( β 0.50 (95% CI 0.09 to 0.92), ) and female gender ( β 1.09 (95% CI 0.15 to 2.02), ) were predictive of higher incisional pain scores at POD#10. A regression analysis was performed to identify secondary factors impacting postoperative pain scores. The primary outcome showed no statistically significant difference on postoperative pain scores between the suture (6.0 (IQR 5.0–8.0)) and staple (7.0 (IQR 5.0–8.0)) cohorts at postoperative day (POD) #1 (adjusted β 0.17 (95% CI −0.61 to 0.95), ). A retrospective review of 155 patients implanted with either a spinal cord or dorsal root ganglion stimulator between 20 was undertaken to determine if the type of surgical closure was related to degree of postoperative surgical site discomfort.

The most efficacious mechanism of surgical closure-specifically a running suture closure compared to a surgical staple closure-is debated. There is a paucity of data related to defining best practices in these specific patient populations, and historically, providers have relied on consensus committees to opine on the best techniques for patient safety and experience. Spinal cord and dorsal root ganglion stimulation are minimally invasive surgical techniques used to treat an array of chronic pain disorders.


 0 kommentar(er)
0 kommentar(er)
